A wireless contact lens that monitors eye pressure and delivers glaucoma drugs on demand has been tested in animals
This device could help treat the eye condition glaucoma by monitoring the build-up of pressure inside the eye and automatically delivering drugs when it rises too high.
Glaucoma affects about 80 million people worldwide according to some estimates and is caused by insufficient drainage of fluid from the eye, which elevates eye pressure and can damage the optic nerve that transmits visual signals to the brain.
The condition is commonly treated using drugs that help drain excess fluid from the eye, administered in the form of eye drops. But people may fail to stick to their treatment schedule, according to Xi Xie at Sun Yat-Sen University in Guangzhou, China, and his colleagues.
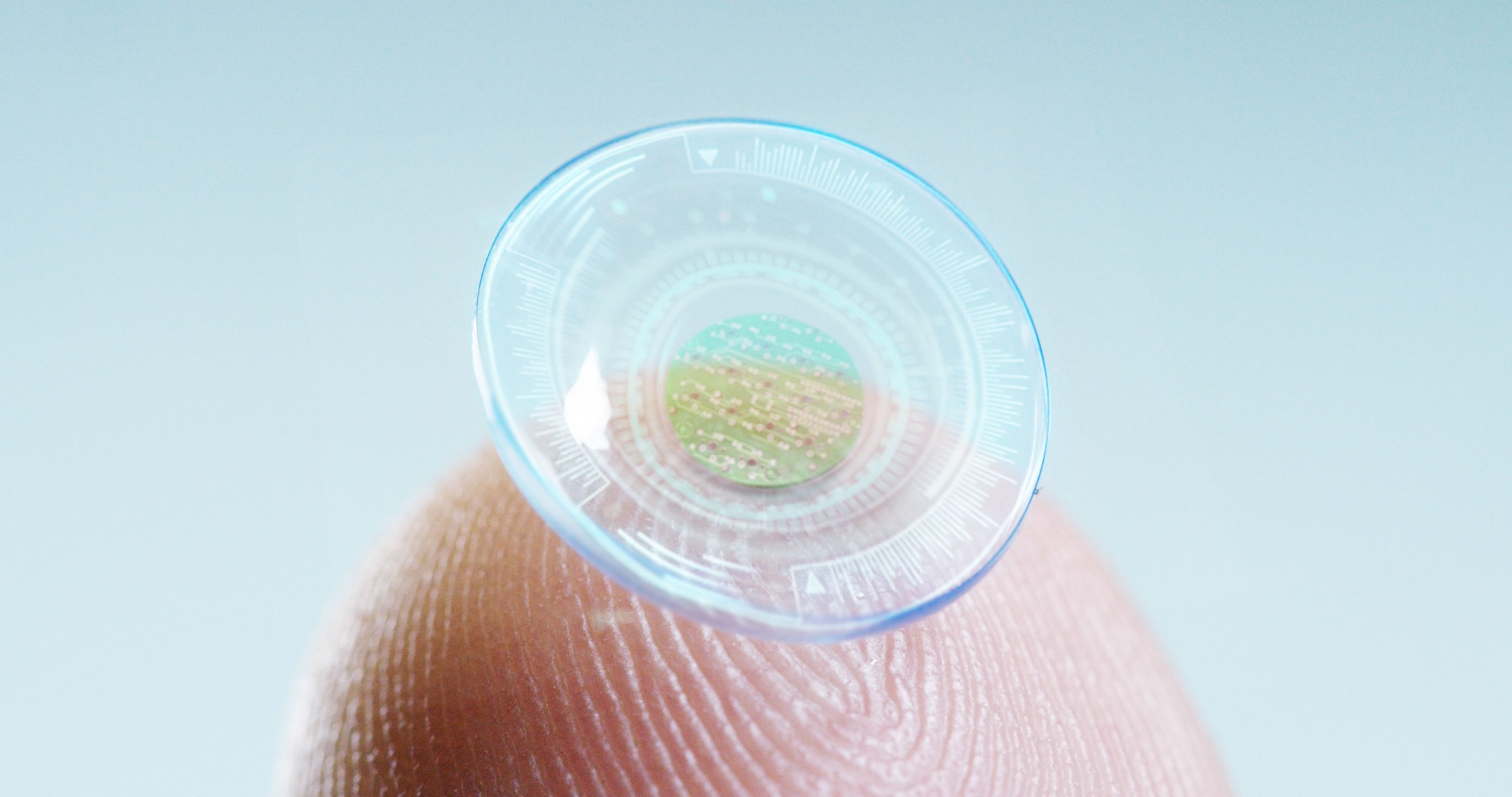
They designed a prototype contact lens device that can sense eye pressure and release glaucoma drugs when needed. The outer layer of the lens has six tiny copper plates arranged in a ring around the pupil that sense eye deformation caused by a rise in eye pressure. An antenna placed near the eye then transmits the data to a nearby computer. The inner layer of the lens – in contact with the cornea region of the eye – is loaded with a pressure-lowering drug called brimonidine that can be released when the lens receives a signal from the computer via the antenna.
The researchers have trialled their lenses in rabbits without glaucoma. They first demonstrated that the device could monitor eye pressure in the animals and transmit the data wirelessly to the external computer. Then they used the computer to wirelessly transmit a signal to the contact lens that triggered the release of brimonidine.
By then tracking the rabbits, they found that the animals’ eye pressure had decreased by around a third after 30 minutes and by more than 40 per cent after 2 hours, on average.
“The realisation of this technology for use at point-of-care settings could revolutionise the lives of millions of patients with glaucoma,” says Ali Yetisen at Imperial College London. “It [would be] a wonderful addition to the [tools] of the ophthalmologist.”
However, further studies will be needed to assess how well the device works in humans.
Source: New Scientist








